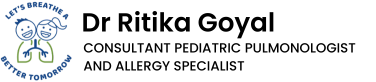
A newborn baby develops noisy breathing on day 3 of life, more prominent when the baby is awake, agitated, crying and almost inaudible when baby is asleep. When the baby is sleeping on his tummy, the noise miraculously goes away and then comes back as soon as he is on his back.
This is a typical presentation of a baby with laryngomalacia. Laryngomalacia is a medical term for babies born with weak cartilages and muscles of the larynx or the voice box or the glottis. This is the part of the airway that works as a trapdoor right at the inlet of lungs, beyond which the trachea or the windpipe begins. As a result the airway inlet is floppy and narrow leading to production of loud noise when the baby inhales.
This condition is absolutely benign and resolves as the baby grows older. By around 1 year of age, 90% of babies with laryngomalacia, outgrow this airway narrowing and have no noisy breathing sounds. However, these babies have to work hard to keep breathing through a narrow airway right from birth and for that they require some special care.
What are the possible problems that a baby with laryngomalacia can have?
Babies with laryngomalacia often have increased work of breathing and parents may notice some chest wall recessions, some recessions in the neck area, especially when the baby is active, playing, agitated or crying.
Gastroesophageal reflux is commonly seen associated with laryngomalacia, causing repeated vomiting, poor weight gain and other feeding issues. y
Some babies may have episodes of apnea or breath-holding, bluish discoloration of skin as a result of transient complete obstruction of the airway.
Poor weight gain and feeding difficulties must be vigilantly monitored for these babies.
In some circumstances, laryngomalacia may be associated with other birth anomalies and therefore, babies must be screened by thorough physical examination or bronchoscopy, if required.
How do we diagnose laryngomalacia?
Diagnosis is mainly clinical although flexible bronchoscopy can be done to confirm the diagnosis of laryngomalacia. Bronchoscopy allows real-time visual assessment of the glottis and surrounding structures. It also helps in visualising the subglottis, trachea and lower airway to rule out any other co-existing airway anomaly.
Flexible bronchoscopy helps assess the severity of airway obstruction based on which treatment can be planned.
Do all children with laryngomalacia need a bronchoscopy?
Laryngomalacia is clinically suspected based on clinical history and physical examination of the baby and owing to its self-remitting nature, a wait-and-watch approach is followed in majority of cases. However, in the presence of following features, flexible bronchoscopy maybe advised
- 1. Fast breathing with chest indrawing
- 2. Oxygen saturation fall
- 3. Episodes of apnea (sudden cessation of breathing)
- 4. Bluish discolouration of skin
- 5. Regurgitation of feeds or gastroesophageal reflux
- 6. Stridor since birth (day 1)
In presence of above mentioned features, the severity of airway obstruction must be assessed.
How do we treat a child with laryngomalacia?
Conservative management (wait-and-watch approach) is usually successful in 90% of babies. As the cartilaginous and muscular structures around the glottis grow and strengthen with age, symptoms of airway obstruction gradually disappear. In less than 10% cases of severe airway obstruction, coexisting airway anomaly, comorbidities like GERD that hamper growth and development, surgical intervention may be advised.
Growth of the baby and developmental milestones are monitored vigilantly in the first year of life. Children with GERD may require anti-reflux measures and frequent growth monitoring.